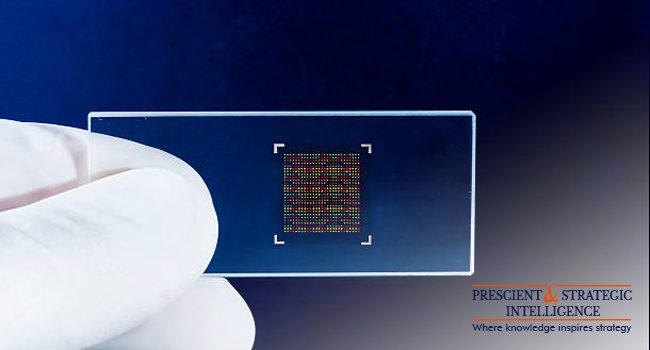
It has not been much time since microarray came to the scene of biotechnology. Scientists can understand the gene functions of any creature by tracking the genes and their products simultaneously, with this technology. It has been considered as one of the finest achievements in science and will revolutionize biology.
Diagnosis and Treatment
The use of microarray in oncology is known almost by everyone. But this is used for the study of inflammatory, cardiovascular, and infectious diseases, along with psychiatric disorders.
Microarray applications can be categorized into different types
- Discovering the Target
The microarray is put to use for comparing diseased cells with healthy cells for discovering the characteristics of a specific disease. This helps in finding the genes responsible for that ailment.
- Drug Discovery and Leads
After the discovery of the target, microarrays are used for screening screen potential compounds and recognize the toxicity of the lead compound that will help in deciding appropriate medication for the patient. The study of antibodies, along with microorganism’s virus and bacteria, also helps in the detection of more efficient antibiotics and vaccines.
- Diagnostics and prognostics:
The microarray is extensively used for knowing the exact stage of a disease, tumor and other vital factors for the patient.
- Pharmacogenomics and Theragnostic
The microarray technique can help you to decide upon the treatment of the patient and therapy based on the genetic makeup of a person. Therefore, it supports in implementation of personalized treatments then making the use of generalized ones. It can also keep in check the side-effects of medications.
Biotech and Other Researches Happening
Microarray can help you identify new genes, and studying their expressions and functions in diverse conditions. It comprises the finding of of the genetic sequence of organisms like humans, mice, and microbes. It also supports in conducting studies in agriculture; for instance, it can be put to use for studies associated with pest control.
Also, oligonucleotide microarray technology used for analyzing exposure of toxic biomarkers. This comes good in classification of toxins into different categories on the basis of responses of the biomarkers and investigate the risk factors in the environment. It can prove its worth in understanding the catabolism of xenobiotics, which has the ability to improve bioremediation procedures with a direct influence on pollution control and environmental organization.
With the usage of species-specific arrays, scientists also conduct studies regarding the evolution of diverse species. This helps in getting more info about genetic mutation and the notion of common ancestry.
Crime and Security
Microarray can detect BWAs. These are toxins or microbes produced by them that are deliberately dispersed by the anti-social elements to for spreading diseases in human and other organisms. The microarray offers a platform providing sensitive, fast, and simultaneous identification of these agents. This is useful for national security.
Also, it is significant in forensic analysis. SNP are put to use in forensic analysis for getting the details of DNA that will be helpful for investigation. The current detection of the abundance of SNPs accompanied by the ease of automation and contraction of the detection techniques has opened the gates for the application of microarray in forensics.
Coming to a Conclusion
There has been an increasing prevalence of cancer all over the world, and this has a positive impact on the demand for microarray analysis. The demand will reach a value of USD 9,011.1 million by the end of this decade.