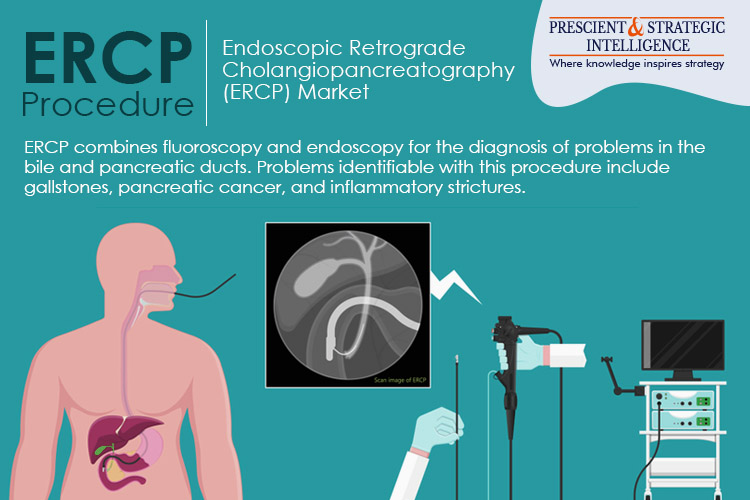
The ERCP procedure, also known as endoscopic retrograde cholangiopancreatography, identifies and addresses issues with the pancreas, liver, gallbladder, and bile ducts. It combines the usage of an endoscope—a flexible, long, lighted tube—with X-ray technology.
Your healthcare practitioner maneuvers the scope via your mouth, neck, stomach, esophagus, and the first segment of the small intestine. Your medical professional can look into these organs to look for any issues. After that, the doctor will insert a tube with a dye within it through the scope.
Application of ERCP
In addition to complex acute and chronic pancreatitis, gallstone pancreatitis also involves ERCP. Randomized studies have demonstrated that ERCP will reduce morbidity and have hinted at a potential reduction in mortality for some individuals with gallstone pancreatitis.
Patients with an affected stone in the main bile duct and people whose gallbladder resection will be postponed are two groups who will benefit from ERCP. Transpapillary stenting is a useful treatment for primary pancreatic duct leakage found by ERCP.
If they connect with the pancreatic duct, symptomatic pseudocysts, walled-off peripancreatic or pancreatic fluid collections observed in acute and chronic pancreatitis may be drained via the papilla. If they don’t, drainage can be done by performing a needle-knife papillotomy to create a cystogastrostomy or cystoduodenostomy.
Transpapillary drainage also affects pancreatic fistulas, openings between the pancreatic duct. Similar methods work well to treat pancreatic ascites, a significant accumulation of abdominal fluid linked to pancreatic duct rupture.
When treating individuals with chronic pancreatitis or recurrent acute, endoscopic retrograde cholangiopancreatography (ERCP) may find tumors, localized pancreatic duct constriction, common bile duct stones, or duct narrowing that cannot be observed with conventional imaging modalities.
Stents are used as a stopgap measure before surgery to treat pancreatic and bile duct strictures. Abdominal pain caused by chronic pancreatitis may occasionally be reduced by removing stones. ERCP can also be used to diagnose and treat pancreatic cancer.
Brush cytology, intraductal biopsy, and fine needle aspiration are a few techniques that may be used to identify pancreatic cancer tissue. Endoscopic ultrasonography has essentially replaced ERCP in detecting this malignancy; however, given the limited sensitivity of duct brushings and the significant morbidity associated with ERCP.
Transpapillary stents have made it easier to address this challenging issue by providing palliative care for biliary blockage. It is still debatable whether biliary and pancreatic sphincterotomy should be used as a therapy option for ERCP-detected occult anatomical or physiological abnormalities.
The ducts from the two embryonic halves of the pancreas, known as the ducts of Santorini and Wirsung, might fail to merge fully, leading to pancreatic divisum. This anatomical variation is common even in those without pancreatitis.
There is conflicting evidence that decompressing one of these ducts can lower the incidence of recurrent pancreatitis. The muscle in a circle called the sphincter of Oddi regulates pancreatic and bile duct discharge.